Trigeminal Neuralgia
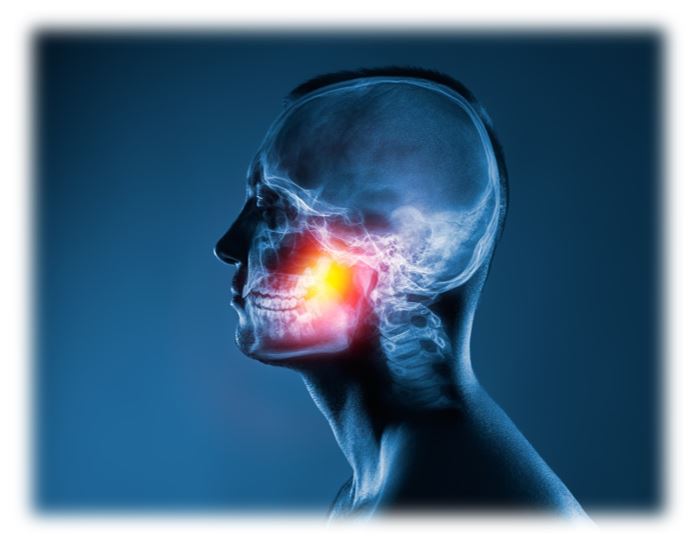
What is Trigeminal Neuralgia?
Trigeminal neuralgia, also known as tic douloureux, is a type of neuropathy or chronic pain condition affecting the trigeminal nerve. The trigeminal nerve is responsible for transmitting sensations from the face to the brain. This disorder is characterized by sudden, severe, and stabbing pain in the face, typically on one side. The pain can be intense and excruciating. And, is often described as sharp, electric shock-like, or burning in nature.
The episodes of pain can be triggered by various factors. These include touching the face, eating, drinking, brushing teeth, talking, or even exposure to wind. Trigeminal neuralgia usually affects one side of the face. However, in some cases, it may occur on both sides.
The condition is thought to be caused by the compression or irritation of the trigeminal nerve as it exits the brainstem. This compression is commonly attributed to a blood vessel pressing against the nerve. But, in some cases, it may be due to a tumor or other structural abnormalities in the area.
Trigeminal neuralgia can be debilitating and significantly impact a person's quality of life. The pain attacks can be frequent and unpredictable. This can lead to anxiety and avoidance of triggers. It is more common in people over 50 years old and is more prevalent in women than in men.
Treatment for trigeminal neuralgia may involve medications to control pain, such as anticonvulsants or muscle relaxants. But, in severe cases or when medications are ineffective, surgical options like microvascular decompression or nerve rhizotomy may be considered.
How Does Ketamine Work to Treat Trigeminal Neuralgia?
Neuropathic pain such as trigeminal neuralgia, often described as shooting, burning, or tingling sensations, can be a debilitating condition resulting from damage or dysfunction of the nervous system. This condition poses a significant challenge to both patients and medical professionals due to its complex and difficult-to-treat nature. An unexpected medication called ketamine has emerged as an alternative with promising therapeutic potential. Originally developed as a general anesthetic in the 1960s, ketamine quickly gained popularity due to its unique characteristics. During its early use, doctors noticed that patients who received ketamine as an anesthetic experienced unexpected relief from chronic pain conditions, including neuropathic pain. This serendipitous discovery prompted researchers to delve deeper into ketamine's potential for treating certain chronic pain conditions.
Understanding Neuropathic Pain
Neuropathic pain arises from the miscommunication between the nerves, spinal cord, and brain. It can be caused by a variety of factors. Theses include nerve injuries, diabetes, viral infections, or chronic diseases like multiple sclerosis. Unlike nociceptive pain, which is the body's normal response to injury, neuropathic pain persists even after the initial cause has healed. Managing neuropathic pain has proven challenging. And, traditional treatments, such as opioids, non-steroidal anti-inflammatory drugs (NSAIDs), and anticonvulsants, often provide limited relief and come with undesirable side effects. Moreover, these treatments do not address the root cause of the pain, leading to long-term reliance on medications.
The NMDA Receptor and Glutamate Signaling
To understand how ketamine works to treat neuropathic pain, we must explore its mechanism of action within the brain. Ketamine acts on a particular receptor known as the N-methyl-D-aspartate (NMDA) receptor. The NMDA receptor plays a crucial role in modulating the transmission of pain signals in the central nervous system. In the context of neuropathic pain, an excessive release of the neurotransmitter glutamate leads to the overactivation of NMDA receptors. This hyperactivity results in increased pain sensitivity and the amplification of pain signals. Ketamine's main role is to block these NMDA receptors, reducing their overstimulation and subsequently dampening pain signals.
Neuroplasticity and Ketamine
Another crucial aspect of ketamine's pain-relieving properties lies in its ability to enhance neuroplasticity. This is the brain's capacity to reorganize and form new neural connections. Chronic pain conditions can cause maladaptive changes in the brain. This can make the pain experience more intense and persistent. Ketamine's impact on neuroplasticity helps to reverse some of these maladaptive changes and promote healthier neuronal connections.
Rapid Onset and Short Duration of Action
One of the remarkable features of ketamine as a neuropathic pain treatment is its rapid onset of action. Unlike traditional analgesics that may take days or weeks to take effect, ketamine often provides relief within minutes to hours after administration. The pain relief from a single ketamine infusion is typically limited to a few days to a week or so. Most patients will require regular treatments that are scheduled based on individual response to the treatment. Some find it beneficial to cluster two or three infusions close together while others use a more regular dosing schedule.
Ketamine Treatment Plan for Trigeminal Neuralgia
Ketamine treatment for trigeminal neuralgia generally requires the administration of multiple IV infusions. This is a case where more ketamine can yield better pain relief. The safest way to infuse more ketamine is by using longer infusion times. Most of our patients receive either 1-hour or 2-hour infusions based on individual response. There can be a trade off between having a longer, more intense infusion or coming in more frequently for shorter infusions. This can be an intense process for some. But, we always proceed one step at a time with safety being the primary concern. The treatment should only be performed by qualified healthcare professionals. And, be administered in a controlled environment due to the risks associated with ketamine use.
Caution and Considerations
While ketamine shows significant promise in treating chronic pain conditions such as trigeminal neuralgia, it is essential to undergo a thorough screening prior to initiating treatment. Most patients can safely receive ketamine therapy. There are a few medical conditions that might require treatment prior to beginning therapy or stop you from receiving this treatment. A few examples are uncontrolled hypertension, active substance abuse, pregnancy or unstable cardiac disease. Ketamine is not a first-line or stand-alone treatment for chronic pain. Ketamine infusion is intended to be one component of a multimodal treatment regimen.
Although the potential for addiction is extremely low, ketamine can be abused or misused. Close monitoring by qualified medical professionals is crucial during ketamine administration to ensure safety and appropriate dosing.
Conclusion
Ketamine's role in treating neuropathic pain presents a beacon of hope for those who suffer from this debilitating condition. It has a unique mechanism of action. The mechanism of action on the NMDA receptor and neuroplasticity sets it apart from traditional analgesics. However, it is essential to acknowledge that ketamine therapy requires close medical supervision. And, it is not suitable for everyone. As research in this field continues to advance, we can hope for more effective and targeted treatments for neuropathic pain. Thus, it improves the quality of life for countless individuals worldwide.
If you have tried other treatments and not found the relief you are looking for, ketamine infusion therapy might be an excellent option for you. Please contact us to schedule a free consultation.
